Medicare Special Enrollment Period After Losing Employer Coverage

-
Last Updated April 2, 2025
When people approach Medicare eligibility, questions often arise about what happens if they lose their health insurance through work. To provide real-world clarity on this topic, professionals with firsthand experience working with Medicare clients shared their insights in response to a single, focused question:
“Am I eligible for a Special Enrollment Period if I lose employer coverage?”
The responses—gathered from a variety of licensed professionals across different regions—shed light on the rules, options, and common pitfalls people face during this transition. Medicare agents and brokers are able to provid a uniquely practical view of how Medicare Special Enrollment Periods work in real-world scenarios.
Confirming SEP Eligibility After Employer Coverage Ends
If you lose your health coverage through an employer, it typically triggers a Special Enrollment Period (SEP), allowing you the opportunity to enroll in Medicare. Across all the responses provided, this was a consistent theme: losing employer coverage is recognized as a qualifying event that opens up an SEP.
In nearly every case, losing job-based coverage grants access to a Medicare SEP, provided the coverage was deemed creditable. Some professionals described this as a life-changing event that initiates eligibility to sign up for Medicare plans. This can include enrolling in various parts of Medicare such as A, B, C, or D. Even if you are over 65 and delayed enrolling in Medicare while covered by an employer plan, the end of that coverage creates an opportunity to enroll without standard penalties.
Several responses emphasized the importance of verifying that the lost coverage was creditable. When your group coverage is creditable, it essentially means it met or exceeded the benefits Medicare offers. This status is often confirmed through your group insurance provider or human resources department. Losing such coverage typically makes you eligible to enroll in a Medicare plan without late penalties.
Some professionals also noted that SEP eligibility can apply in a range of other situations beyond job loss—such as moving to a new state or being affected by a natural disaster—though the context here specifically relates to losing employer coverage. Regardless of circumstance, a SEP becomes available when that loss occurs.
Enrollment Timeframes: How Long You Have
When you lose your employer-based health insurance, you don’t have unlimited time to act. The responses you provided included a few variations on the SEP time window, but all emphasized that there is a defined and limited period in which you can make your Medicare selections.
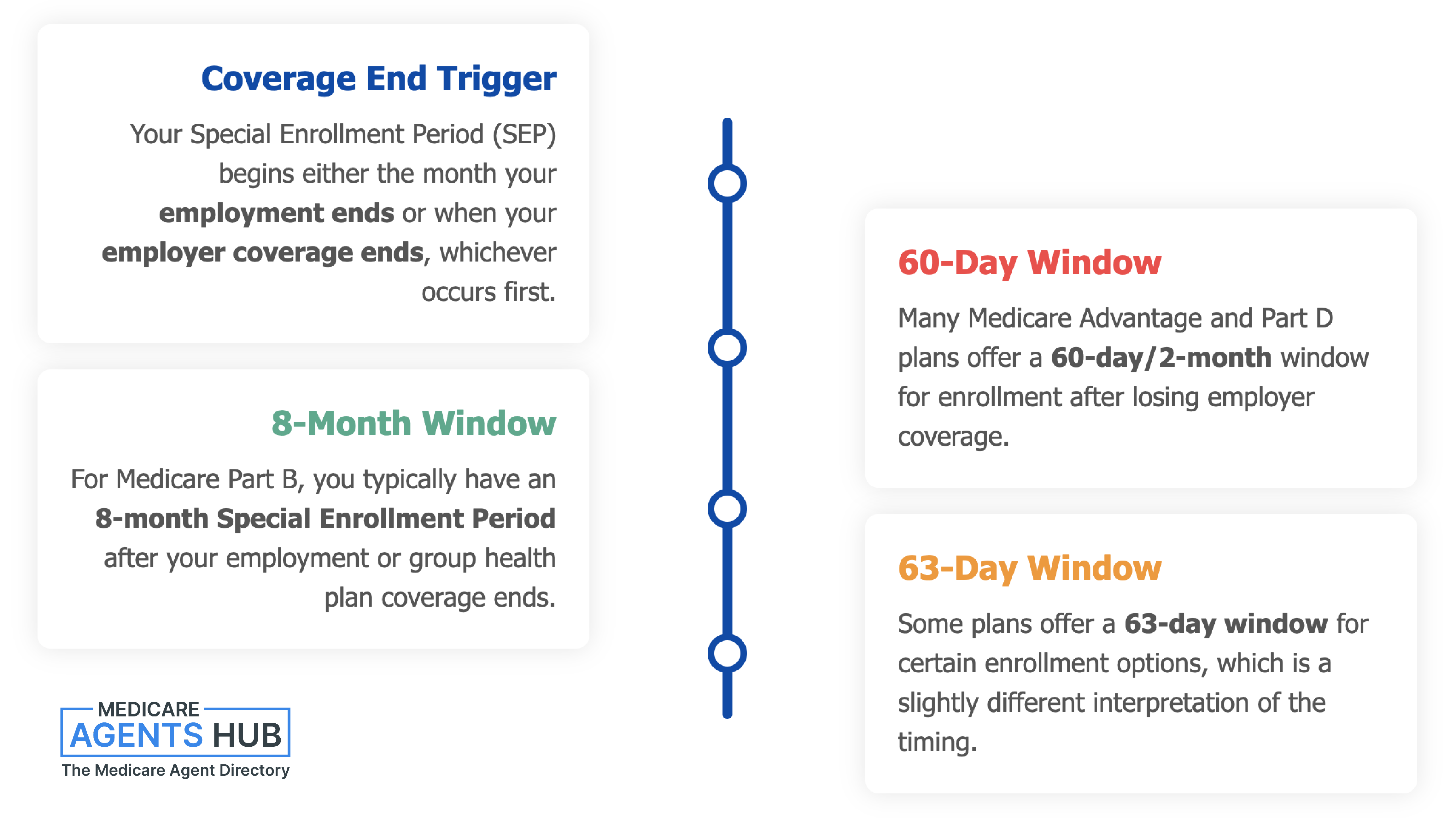
Several agents stated that you have a 2-month or 60-day window to enroll in Medicare after losing employer coverage. Others mentioned an 8-month SEP, depending on which parts of Medicare you are looking to enroll in. One response noted a 63-day window, adding a slightly different interpretation of the timing. A few also pointed out that your enrollment period may begin either the month your employment ends or the month your employer-sponsored coverage ends, depending on which occurs first.
Despite the different numbers provided, all professionals highlighted the same core idea: you must act quickly to ensure continuous coverage and avoid any potential penalties or delays. Waiting too long could result in a gap in your healthcare or prescription drug coverage, and that can complicate matters significantly.
Some also noted that while Medicare does give you a few months to act, it’s best not to wait until the deadline approaches. Prompt coordination ensures you’re not left uncovered for any period of time.
Enrollment Options During SEP
Once your Special Enrollment Period begins, you gain access to a range of Medicare options. Multiple responses described the variety of plans you can choose from, depending on your needs and situation.
You may choose to enroll in Original Medicare, which includes Part A (hospital insurance) and Part B (medical insurance). From there, you can add on a Part D plan for prescription drug coverage. Alternatively, you may opt for a Medicare Advantage Plan (Part C), which bundles coverage into one plan and often includes drug benefits.
Some noted that during this SEP, you're not limited to just enrolling in Medicare itself—you can also select a Medigap (supplement) plan to help cover out-of-pocket costs or change between Medicare Advantage plans if needed.
A few professionals clarified that even if you delayed Medicare Part B initially because you had employer coverage, this SEP allows you to activate it without facing a penalty. Several mentioned that decisions made during this period can determine the trajectory of your healthcare in retirement, reinforcing the importance of evaluating all available plan types.
Additionally, a couple of responses referred to the possibility of coordinating enrollment into multiple parts—such as Parts A, B, C, and D—all at once, depending on the needs of the individual. The takeaway was clear: this is a key window of opportunity to choose or change your Medicare path.
The Role of Creditable Coverage
A recurring concept throughout the responses is the importance of your previous employer coverage being creditable. This term came up several times and plays a critical role in determining your eligibility for a Special Enrollment Period and avoiding late penalties when transitioning into Medicare.
Creditable coverage essentially refers to employer-sponsored insurance that is considered at least as comprehensive as Medicare’s standard benefits. If the coverage you had through your job meets this standard, losing it will open the door to a SEP where you can sign up for Medicare Parts A and B, and make decisions about Advantage plans, Part D, or Medigap coverage.
One insight clarified that the determination of creditable coverage is typically provided by the group insurance provider or your employer’s human resources department. This official confirmation helps ensure that you are eligible for the SEP and that you won’t be penalized for delayed Medicare enrollment. It’s a vital step in the process, especially for individuals who delayed enrolling in Medicare Part B while they were still working.
Several responses stressed that creditable coverage status must be clear at the time of losing your job-based plan. Without that confirmation, the ability to access SEP benefits could be compromised or delayed, leading to confusion or potential penalties. Therefore, verifying the creditable status of your previous coverage is one of the most important things to do immediately after leaving your job.
COBRA and Medicare: A Cautionary Note
While COBRA coverage might seem like a convenient extension of employer-sponsored insurance, it came up in multiple responses as a potential pitfall in the context of Medicare eligibility and SEP rules.
A few professionals cautioned that COBRA is not considered creditable coverage under Medicare. This distinction is crucial. If someone chooses COBRA instead of enrolling in Medicare during their SEP, they may unknowingly forfeit their right to penalty-free enrollment and could be left with gaps in coverage.
One contributor pointed out that Medicare does not view COBRA as a qualifying substitute, which means that relying on COBRA during this transition can prevent you from making full use of your SEP. Even if you still have access to healthcare through COBRA, Medicare may not consider you “covered” in the same way it does for employer-sponsored insurance, leading to complications down the line.
Additionally, it was noted that COBRA can be significantly more expensive than Medicare options. A few responses suggested that in most cases, it’s financially unnecessary to pay for COBRA when Medicare is available. There was also a strong suggestion to avoid overspending on COBRA, unless your situation clearly calls for it.
In summary, the general advice was to steer away from using COBRA as a bridge to Medicare. Instead, it's usually better to move directly into Medicare during your SEP to avoid penalties and simplify your coverage path.
SEP Rules Vary Based on Circumstances
While the focus here is on losing employer coverage, it's worth noting that several responses highlighted how Special Enrollment Period rules can vary depending on the situation. In other words, while losing job-based insurance is one well-known trigger, there are other life events that may qualify someone for a SEP as well.
A few responses mentioned other scenarios such as moving to a different location or experiencing a weather-related disaster. These events can also trigger a SEP, though the timing and options may be different based on individual factors and, in some cases, state-specific regulations.
Some noted that SEP windows differ slightly depending on what you’re enrolling in—for example, there may be separate timeframes for enrolling in Medicare Parts A and B versus Medicare Advantage or prescription drug plans. One explanation also pointed out that the window for enrolling in Part A and B might be longer than the one for Advantage or drug plans.
There were reminders that SEP eligibility isn't always the same across all circumstances, and some emphasized the importance of checking your specific situation to understand how long you have and what you’re allowed to do. SEP guidelines can be influenced by your location, plan availability, and other variables unique to your situation.
These nuances reinforce the value of personalized guidance during this transition. While losing employer coverage is a common SEP trigger, how you respond—and what rules apply—may vary based on the details of your life and benefits history.
Coordinating with Brokers for Seamless Transitions
Navigating Medicare enrollment during a SEP can be confusing, especially if you're dealing with deadlines, multiple plan options, and coverage transitions. Several responses recommended working with an experienced broker who can guide you through the steps and minimize the risk of a coverage gap.
Some contributors emphasized that brokers are skilled at helping individuals understand their SEP options and plan benefits, as well as making the process faster and more seamless. For example, coordinating plan start dates to ensure continuous care and medication coverage was mentioned as an area where expert help can be especially valuable.
There were insights suggesting that even though Medicare grants a SEP, it's not always easy to know what to do without assistance. The options—Original Medicare, Advantage plans, Medigap, drug plans—all come with their own enrollment rules and timelines. A broker can help you navigate those differences and avoid mistakes.
A few responses also advised against trying to go through this transition alone, especially if you are unsure about plan compatibility, eligibility timing, or how to submit enrollment paperwork correctly. Support from someone who knows the ins and outs of Medicare can make a meaningful difference.
Ultimately, getting help from a broker isn’t just about saving time—it can also help ensure that your transition is smooth, strategic, and properly aligned with your healthcare goals.
Conclusion: You Get Access to Medicare Without Late Penalties
Losing your employer coverage is a major life transition—and fortunately, it often opens the door to a Special Enrollment Period that gives you access to Medicare without late penalties. Every professional who weighed in agreed: this is a critical opportunity that must be acted on quickly and strategically.
Your SEP window may be as short as 60 days or extend to 8 months depending on what parts of Medicare you’re enrolling in. It's essential to confirm that your prior insurance was creditable, avoid leaning on COBRA unless necessary, and explore your plan options thoroughly. There’s also flexibility in the system—SEPs can vary based on your circumstances, and getting support from a knowledgeable broker can help you take full advantage of your options.
The choices you make during your SEP will shape your future healthcare experience. Taking informed, timely steps will set you up with the coverage you need—without unnecessary costs or delays.