Medicare in 2025: Must-Know Changes and Challenges for New and Current Enrollees

In 2025, Medicare is undergoing transformative changes that are sparking conversations among those aging into the program and current enrollees alike. From groundbreaking cost-saving measures to concerns about privatization, these shifts are reshaping how beneficiaries plan for healthcare. As someone passionate about helping others navigate Medicare, I’ve compiled the top trending topics you need to know, drawing from recent updates and discussions, with insights tailored for both new and existing enrollees.
1. The Game-Changing $2,000 Cap on Part D Drug Costs
Starting January 1, 2025, the Inflation Reduction Act introduces a $2,000 annual out-of-pocket cap on prescription drug costs for Medicare Part D plans, including those bundled with Medicare Advantage. This reform eliminates the infamous "donut hole," where beneficiaries once faced steep costs. An estimated 3.2 million enrollees could save an average of $1,500, with some, especially those on pricey medications like cancer drugs, saving up to $3,000 or more.
For You: If you’re aging into Medicare, this cap makes Part D plans more predictable, especially if you manage chronic conditions requiring costly drugs. Current enrollees with high drug expenses should review their plans during open enrollment (October 15–December 7, 2024) to ensure their medications are covered under the cap, as it only applies to drugs on a plan’s formulary.
However, watch out: insurers may raise premiums or tweak formularies to offset these costs, so compare plans carefully.
2. Smoothing Costs with the Medicare Prescription Payment Plan
A new voluntary Medicare Prescription Payment Plan, launching January 1, 2025, lets Part D enrollees spread out-of-pocket drug costs over the year. This is a lifeline for those hit with high early-year expenses or short-term costly prescriptions.
For You: New enrollees can budget more effectively, avoiding the shock of large upfront costs. If you’re already on Medicare, this plan could ease the burden of variable drug expenses, though it doesn’t lower total costs—just distributes them. Be aware that opting in may feel complex, and awareness of this option is still growing.
3. Medicare Advantage: Fewer Plans, Shifting Networks
In 2025, Medicare Advantage (MA) plans are shrinking, with an average of 34 plans per county (down from 43 in 2024). Some health systems, like Essentia Health and Sanford Health, are dropping MA plans such as Humana and UnitedHealthcare due to prior authorization hurdles and high denial rates. Plus, some MA plans are cutting supplemental benefits—like gym memberships or over-the-counter medication allowances—to manage costs from the Part D cap and reduced government payments.
For You: If you’re new to Medicare, choosing between Original Medicare and MA is trickier with fewer plans and changing provider networks. Current MA enrollees, especially the 1.4 million in terminated plans, should check their Annual Notice of Change (ANOC) to confirm in-network doctors, hospitals, and benefits like dental or vision. Don’t get caught off guard—review your options now.
4. Rising Premiums and Cost-Sharing for Parts A, B, and D
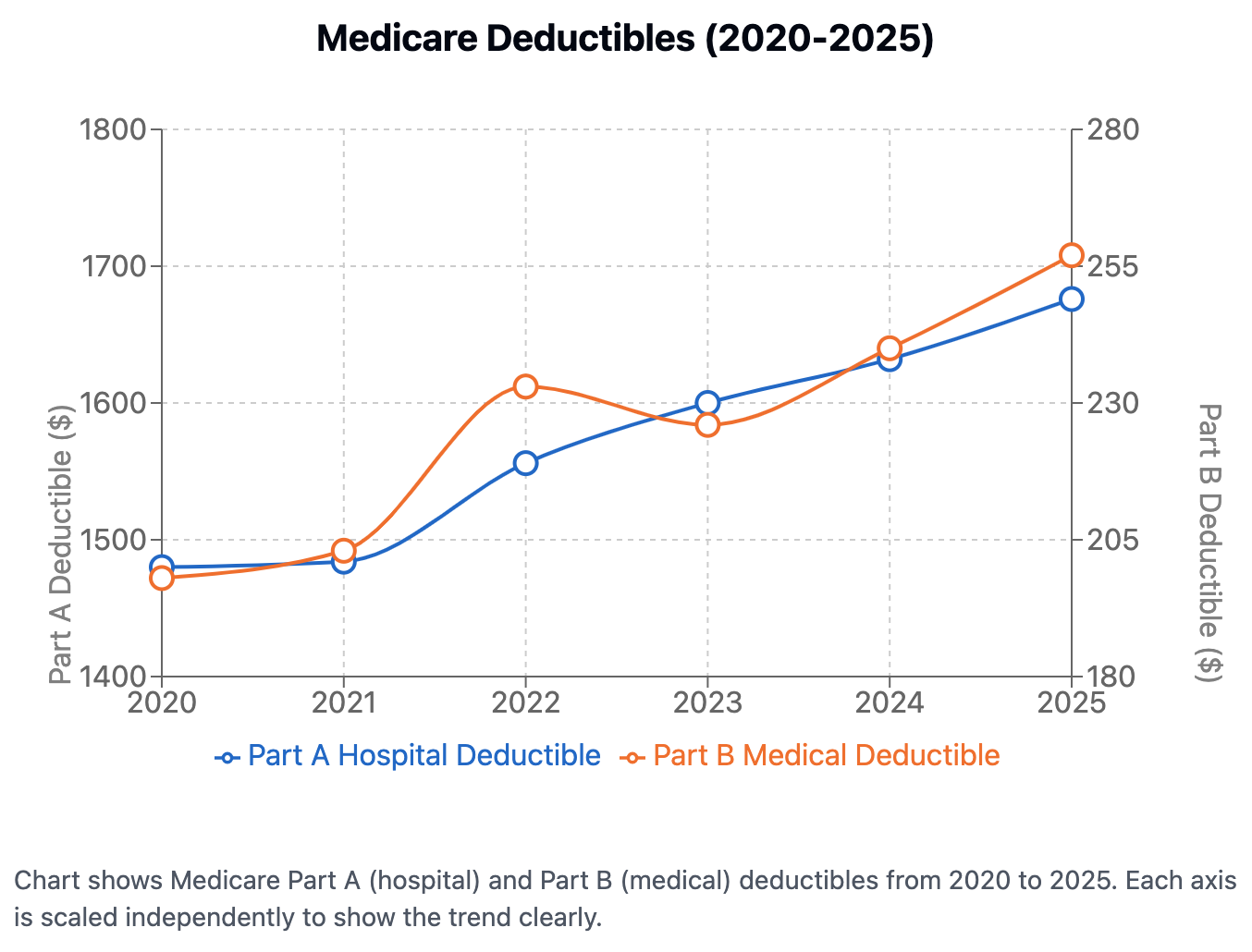
Medicare costs are climbing in 2025. Part B premiums are up to $185/month (a $10.30 increase), with deductibles rising to $257 (up $17). Part A hospital deductibles are $1,676 (up $44), and Part D deductibles can hit $590 (up from $545). High earners (above $106,000/year) face steeper income-related adjustments (IRMAA), impacting about 8% of beneficiaries.
For You: If you’re aging into Medicare, factor these costs into retirement planning, especially if you don’t qualify for premium-free Part A (requiring 40 quarters of work). Current enrollees on fixed incomes may feel the pinch, though the 2.5% Social Security COLA for 2025 offsets the Part B hike for most. High-income retirees should review IRMAA thresholds to manage expenses.
5. Expanded Benefits and Support Programs
Medicare is broadening its reach in 2025, covering more mental health services, cardiovascular risk assessments, and dental care for specific treatments. The Guiding an Improved Dementia Experience (GUIDE) program is quadrupling, offering caregiver support, 24/7 helplines, and respite care. Caregiver training and hospice respite care are also newly covered. The Extra Help program for low-income beneficiaries is easier to access, covering most drug costs for those below 150% of the federal poverty level.
For You: New enrollees with chronic conditions or caregiving duties can benefit from these enhancements, especially in MA plans with supplemental coverage. Current beneficiaries should explore Extra Help (e.g., $4.90 for generics, $12.15 for brand-name drugs) and GUIDE for dementia care, though low awareness may mean you need to dig for details.
6. Privatization Fears: The Project 2025 Debate
Project 2025, a Heritage Foundation policy agenda, proposes making Medicare Advantage the default enrollment option, fueling fears of Medicare privatization. Critics warn this could limit provider choices, increase prior authorization denials, and add $2 trillion in wasteful spending over a decade if MA enrollment hits 75%. Social media is buzzing with concerns about higher drug prices and reduced care access.
For You: If you’re new to Medicare, weigh MA’s restrictions (like limited networks) against Original Medicare’s flexibility. Current MA enrollees might reconsider plans during open enrollment, fearing future shifts that could curb Traditional Medicare access. These proposals aren’t policy yet, but they’re worth watching.
7. The Long-Term Care Misconception
A recent poll revealed that 49% of adults aged 50–64 and 66% of those 65+ wrongly believe Medicare covers long-term nursing home care—it doesn’t. This misconception is driving calls for better education and planning.
For You: If you’re aging into Medicare, start exploring long-term care options like Medicaid or private insurance now. Current beneficiaries frustrated by this gap should look into alternatives, as social media reflects growing discontent with Medicare’s limitations.
A Critical Take: Opportunities and Risks
The $2,000 Part D cap and payment plan are hailed as cost-savers, but they may trigger higher premiums or reduced MA benefits as insurers adapt. The push toward MA under proposals like Project 2025 raises valid privatization concerns, though evidence on MA’s quality versus Traditional Medicare is mixed—some studies show similar outcomes, others highlight MA’s restrictive practices. The long-term care misconception underscores Medicare’s complexity and the risk of misinformation, which could leave beneficiaries unprepared.
As we navigate these changes, my advice is clear: whether you’re new to Medicare or a seasoned enrollee, stay informed, compare plans diligently during open enrollment, and don’t hesitate to seek help from Medicare.gov or a trusted advisor. The landscape is shifting, but with the right knowledge, you can make choices that protect your health and wallet in 2025.
About the Author: Douglas Carney is a Medicare Broker Licensed in FL, GA, NC, OK and TX.
