How to: Qualify for Medicare’s Special Enrollment Period

-
May 3, 2025
If you missed your initial Medicare enrollment window or the annual Open Enrollment Period, don’t worry, there’s still a way to get covered. Medicare offers Special Enrollment Periods (SEPs) that let you sign up or make changes to your coverage when certain life events occur. These SEPs help you avoid penalties and ensure you have the right coverage when your circumstances change.
What Is a Special Enrollment Period?
A Special Enrollment Period is a time outside the standard enrollment windows when you can enroll in or change your Medicare coverage due to specific life events. These events might include losing other health coverage, moving to a new area, or other qualifying situations. The timing and duration of your SEP depend on the specific event that qualifies you.
Common Reasons You Might Qualify for an SEP
✅ Losing Employer or Union Coverage
If you're 65 or older and lose your employer or union health coverage, you have an 8-month SEP to enroll in Medicare Part B without facing a late enrollment penalty. This period starts the month after your employment or coverage ends, whichever comes first.
✅ Moving to a New Area
Relocating can impact your Medicare coverage, especially if you have a Medicare Advantage (Part C) or Part D prescription drug plan. If you move to a location outside your plan's service area, you qualify for an SEP to switch to a plan available in your new area.
An answer from an agent explains…
"When you move out of a service area, whether from one county to another, or a different state, you must change plans if you have a Medicare Advantage (MA) or Prescription drug plan (PDP). The ability to change plans after a move falls under a Special Enrollment Period (SEP)."
It's crucial to notify your plan provider about your move. If you inform them before moving, your SEP begins the month before your move and lasts for two months after. If you notify them after moving, your SEP starts the month you inform them and continues for two months.
✅ Losing Other Creditable Coverage
If you lose other creditable prescription drug coverage (like from an employer or union), you have a 63-day SEP to enroll in a Medicare Part D plan without penalty.
✅ Changes in Medicaid Eligibility
If you qualify for both Medicare and Medicaid and experience changes in your Medicaid eligibility, you may be eligible for an SEP to adjust your Medicare Advantage or Part D coverage.
✅ Other Life Events
Other situations that may qualify you for an SEP include:
-
Being released from incarceration
-
Losing coverage through no fault of your own
-
Your plan's contract with Medicare ends
Understanding Guaranteed Issue Rights
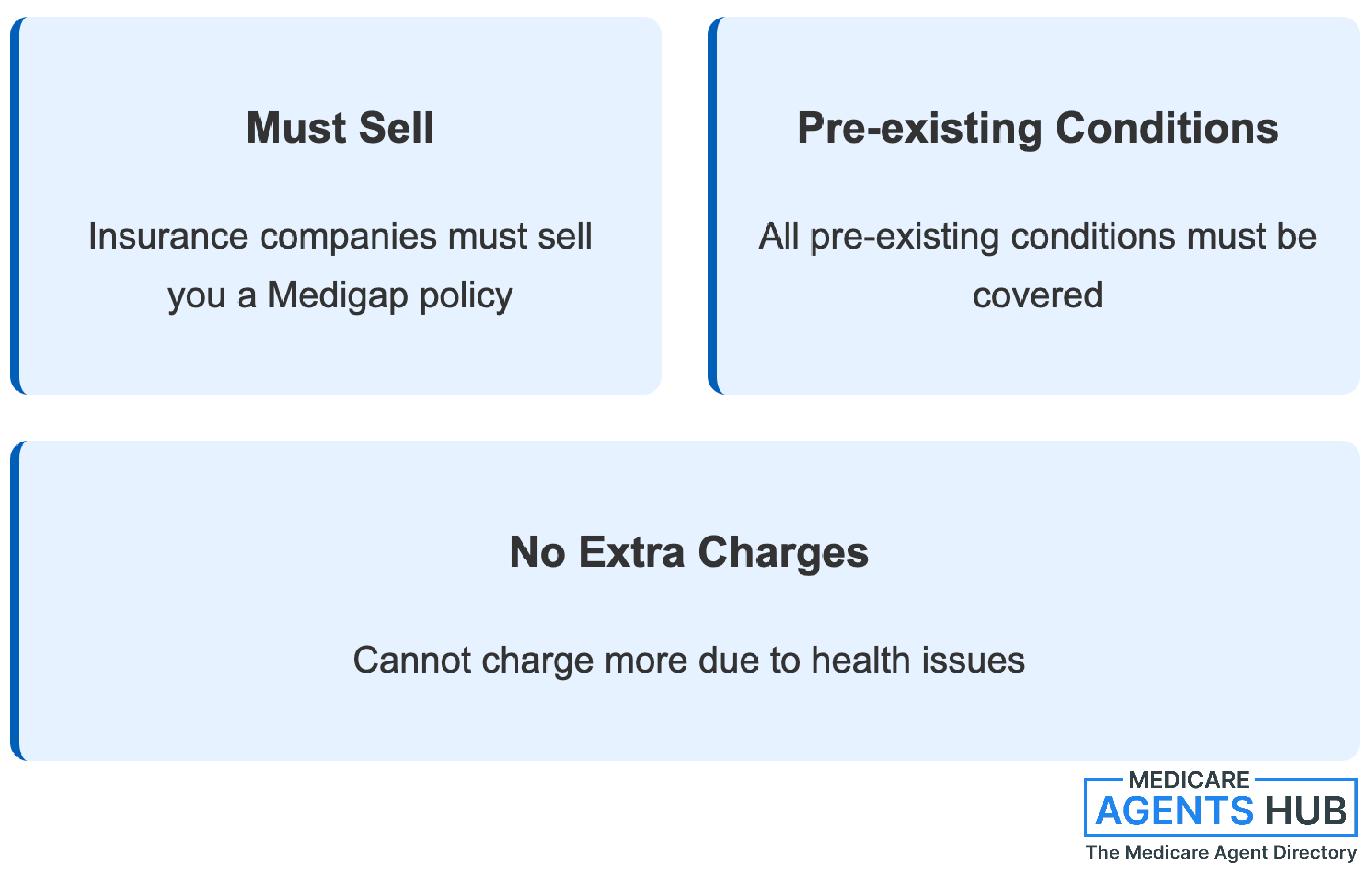
Guaranteed issue rights protect you when buying a Medigap (Medicare Supplement) policy. These rights mean insurance companies must sell you a Medigap policy, cover all your pre-existing conditions, and can't charge you more due to health issues.
While the Medigap Open Enrollment Period is a one-time, six-month window starting when you're 65 and enrolled in Part B, there are situations where guaranteed issue rights apply outside this period. For example, if you lose other health coverage or your Medicare Advantage plan ends, you may have a guaranteed issue right to buy a Medigap policy.
In an answer to a question about Guaranteed Issue John Lopez adds:
"Guaranteed Issue is available for up to 6 months after your Part B becomes effective, and it doesn't have to coincide with the Medicare Open Enrollment Period. There are also other situations in which Guaranteed Issue applies, but consult with a local independent health broker to determine if your situation applies."
Steps to Take If You Qualify for an SEP
-
Identify Your Qualifying Event: Determine the life event that makes you eligible for an SEP.
-
Mark Your Calendar: Note the start and end dates of your SEP to ensure you act within the allowed timeframe.
-
Review Your Options: Compare available Medicare plans in your area to find the best fit for your needs.
-
Enroll Promptly: Sign up for or change your Medicare coverage within your SEP to avoid penalties or coverage gaps.
-
Seek Assistance: If you're unsure about your options, consider consulting a licensed Medicare agent or visiting Medicare.gov for guidance.
Final Thoughts
Life changes can impact your healthcare needs, and Medicare's Special Enrollment Periods are designed to provide flexibility during these times. By understanding the qualifying events and acting promptly, you can ensure continuous and appropriate coverage without unnecessary penalties.
Remember, staying informed and proactive is key to making the most of your Medicare benefits.