Helping Clients Understand Their ANOC: A Resource for Insurance Agents

-
May 15, 2025
Each fall, Medicare Advantage and Part D plan members receive a document called the Annual Notice of Change (ANOC). It’s one of the most important communications they’ll get all year. Unfortunately, many beneficiaries ignore it, skim it, or misunderstand it altogether.
As an insurance agent, a key part of the job is not just to sell a plan - it’s to guide clients through the fine print. The ANOC is where much of that fine print lives. This article will give you a clear, actionable approach to helping your clients understand their ANOC and make informed decisions before the Medicare Annual Enrollment Period (AEP).
What Is an ANOC?
The ANOC is a required document that Medicare Advantage (MA) and Part D plans send to their members by September 30 each year. It details any changes in:
-
Benefits
-
Costs (including premiums, copays, and deductibles)
-
Drug coverage and formularies
-
Provider networks
These changes go into effect January 1 of the following year.
Why Clients Struggle With It
Most clients don’t read their ANOC thoroughly, if they open it at all. The document tends to be lengthy and filled with complex insurance jargon, which makes it intimidating and easy to ignore. On top of that, many clients confuse it with other similar mailings, like the Evidence of Coverage (EOC), and assume it’s just more paperwork. There's also a common belief that if the plan is still active, nothing important has changed and no action is necessary. Unfortunately, this mindset can lead to overlooked cost increases, new restrictions, or changes in drug coverage or provider networks that could significantly impact their care, often not discovered until the new year rolls around and it’s too late to make changes.
Your Role: Make It Simple
Here’s how you can break the ANOC down for clients in a way that’s easy to understand and act on:
1. Start With the Basics
Explain what the ANOC is and why it matters, in plain English.
“This is the document that tells you if your plan is changing next year. It could mean different prices, different doctors, or changes to what’s covered.”
2. Highlight Key Sections
Help clients focus on the most impactful parts:
-
Premiums and Deductibles – “Is your monthly premium going up?”
-
Copays – “Are doctor or hospital visits going to cost more?”
-
Drug Coverage – “Did they remove or re-tier any of your medications?”
-
Provider Network – “Is your doctor or hospital still in-network?”
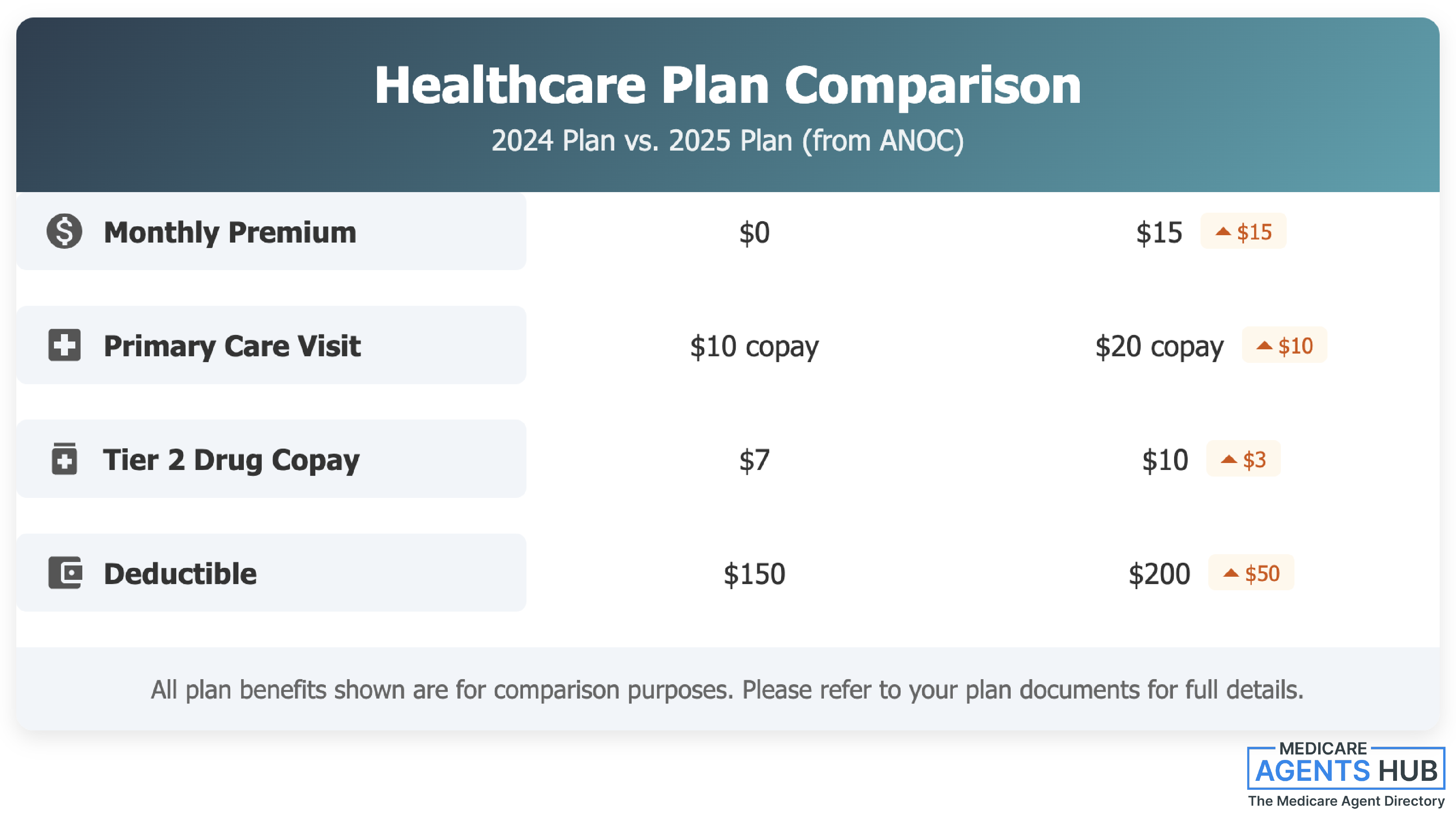
You can even use a simple comparison chart to make changes clearer:
3. Ask Targeted Questions
Don’t just go through the ANOC line by line. Ask specific questions that tie changes to their daily life:
“Do you still take these medications?”
“How often do you visit your specialist?”
“Has your doctor or pharmacy changed recently?”
This helps connect the dots between plan changes and real-world impact.
Be Proactive, Not Reactive
The ANOC should kick off your client outreach in September or early October. Waiting until AEP (Oct 15–Dec 7) to discuss plan changes can limit their options.
Consider these strategies:
💬 Send reminders:
Let clients know to expect the ANOC in the mail and ask them to keep it.
👥 Offer ANOC reviews:
Schedule short calls or meetings to walk through the key points.
📄 Have materials ready:
Comparison charts, FAQs, and simple “What Changed?” summaries go a long way.
Wrap-Up: Keep It Client-Focused
Helping clients understand their ANOC isn’t about impressing them with your knowledge, it’s about making sure they’re in the right plan for the year ahead. By simplifying the language, highlighting what matters most, and offering personalized support, you turn a confusing government document into a powerful tool for client trust and retention.
When clients feel informed, they feel empowered. And when they’re empowered, they stick with the agent who helped them get there.